With increased awareness and improved diagnosis, the number of people with Keratoconus referred to specialists is on the increase. Early diagnosis is ideal because treatment in the form of corneal collagen cross linkage (or CXL) may be more effective the earlier it is performed and because visual rehabilitation is far easier. Optometrists are in a good position to pick up Keratoconus so regular sight checks in the teenage years if vision is changing or myopia (short-sightedness) or astigmatism is increasing should be arranged. In this series of blogs we will look at different aspects of the condition and its treatment. Explanatory animations are available on other parts of the website and links to other educational events will be posted.
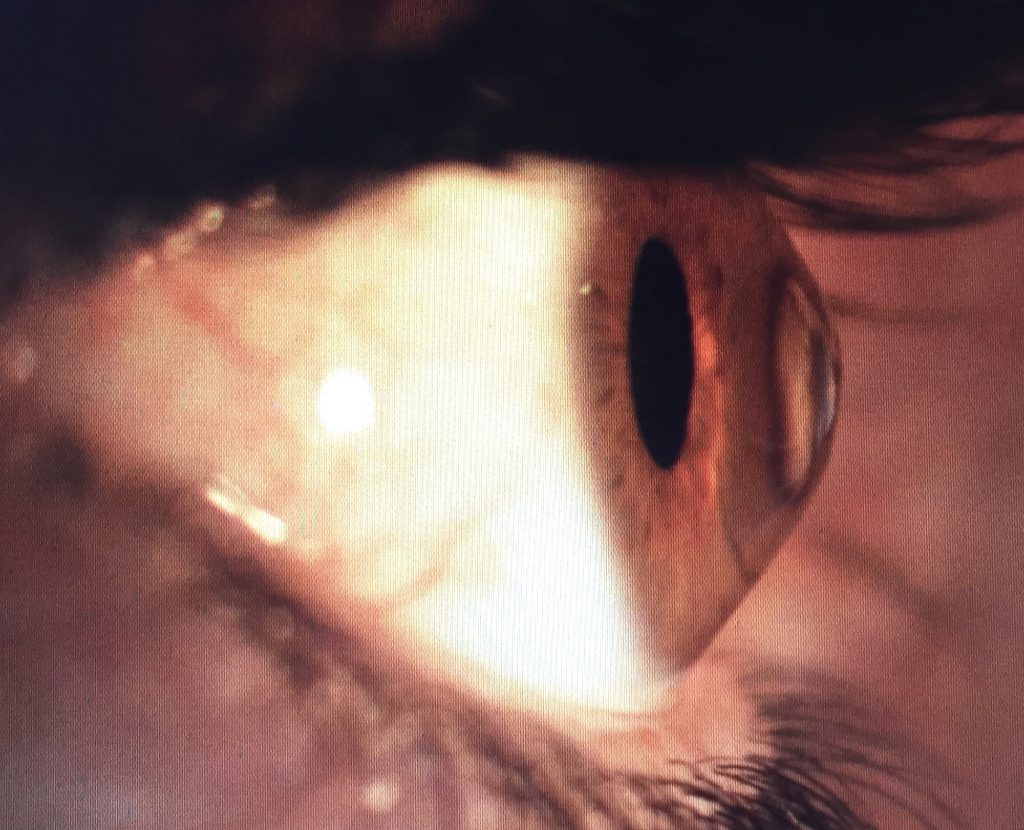
Image of eye affected by Keratoconus
What is keratoconus?
Keratoconus is a condition that affects the cornea which forms the front, transparent, protective coat of the eye.
The cause of KCS is not fully understood but genetics almost certainly plays a part. It is made worse by, but not caused by rubbing the eyes and often linked to allergic conditions such as hay fever, eczema and asthma.
KCS tends to affect both eyes but one eye may sometimes be much worse than the other so that the condition is often asymmetric. Very early KCS is sometimes referred to as Forme Fruste KCS so that vision may be affected in one eye but normal in the other.
The number of new patients diagnosed with KCS varies from 1 person in every 1500 to 1 person in 450 in certain populations. Most people first become aware of changes in their sight in their early teens to twenties. The condition usually stabilizes by the late 20’s and 30’s although some people may experience a later onset of symptoms or stabilization later in their 30’s of 40’s.
The visual symptoms of KCS are caused either by progressive distortion of the cornea leading to increasing regular and irregular astigmatism or in later stages by corneal scarring.
What are the symptoms of KCS?
Vision initially becomes more blurred particularly in the distance and at night or in twilight. People with KCS may notice that figures or text on a screen such as a mobile phone may appear increasingly blurry or appear to have a ghost image. With progression, patients often describe sensitivity to glare e.g. bright sunshine or oncoming car headlights when driving at night. Sources of lights can often seem to be surrounded by haloes or streaks. These symptoms are caused by increased irregularity in the shape of the cornea.
How can Keratoconus be picked up?
An Optometrist will typically notice a change in the spectacle prescription with increasing myopia, astigmatism and altered light reflexes from the cornea during routine sight testing.
Specialist Ophthalmologists will combine clinical examination and corneal topography to reach a definitive diagnosis and can use techniques such as digital subtraction of scan images to look for subtle signs of progression. They will also look for other related conditions such as asthma, eczema and hay fever so that they can treat the individual comprehensively.
What treatments are available for KCS?
Initially visual correction can be achieved with spectacles but as the condition progresses, patients often need to wear contact lenses to achieve good vision. If progression is not halted, surgery in the form of a corneal transplant may be required in up to 20% of those affected.
More recently, corneal collagen cross linkage (aka CXR, C3R, KXL) has been shown to be safe and effective in the treatment of KCS in the majority of cases. CXL was approved by the National Institute for Health and Care Excellence and can be performed as an outpatient procedure taking around 20 minutes.
Collagen Cross linkage is designed to prevent KCS progressing and so early diagnosis of the condition and monitoring with corneal topography is essential.
Other forms of treatment for KCS are designed to improve vision and are typically performed when the condition has stabilized naturally or after stabilization with CXL has been achieved. Treatments include the use of plastic ring segments inserted into the cornea (intrastromal corneal rings, ICR’s) or topography guided (T-CAT) or wavefront laser vision correction. Other treatments which have been used to improve vision in KCS include implantable collamer lens (ICL) surgery and cataract surgery with toric intra-ocular lenses.
Although CXL is primarily designed to stabilize KCS, treatment itself may cause flattening of the conical cornea and influence vision.
Treating allergic eye disease such as allergic conjunctivitis is particularly important in the overall welfare of the patient and will be covered separately.
Background
David Anderson has been practicing Ophthalmology for more than 20 years and has specialized in the treatment of patients with complex corneal conditions including KCS for 15 years. David has been treating KCS patients with CXL since 2010 and is considered to be an expert in managing this condition. David recommends the Avedro Accelerated KXL System (www.avedro.com) available at the Nuffield Hospital Wessex for the treatment of progressive KCS.
Public open evening on Keratoconus
David will be holding an open event to discuss KCS as part of Eye Health Month at Nuffield Hospital Wessex on Wednesday 22nd June 2016. To register for the event please click here.
Medical Disclaimer
This article is for information purposes only and should not be considered medical advice. If you or any other person has a medical concern, you should consult with your health care provider or seek other professional medical treatment. Never disregard professional medical advice or delay in seeking it because of something that you have read on this blog, website or in any linked materials.