Menu
David Anderson performs a wide range of specialist surgical procedures to the cornea including the selective corneal transplant surgeries DSEK, PK and DALK.


The cornea is the transparent dome of tissue that forms the front protective coat of the eye. It is responsible for the majority of the focusing power of the eye. Any condition that reduces the transparency of the cornea will result in loss of vision.
David Anderson completed two full Fellowships in corneal surgery at Moorfields Eye Hospital in London and a one year post-Doctorate at Bascom Palmer Eye Institute in Miami as a TFC Frost Scholar, studying reconstructive techniques including the use of amniotic membrane for complex conditions. He has written and presented extensively on the subjects and has led the Corneal Fellowship programme at University Hospital Southampton for over a decade.
Corneal transplant surgery involves selectively replacing that part of the cornea damaged by disease with healthy tissue from a donor eye e.g. the endothelium in Fuchs’ Dystrophy, or the stroma in Keratoconus. In some cases, all layers of the cornea require replacement by full thickness or Penetrating Keratoplasty (PK).
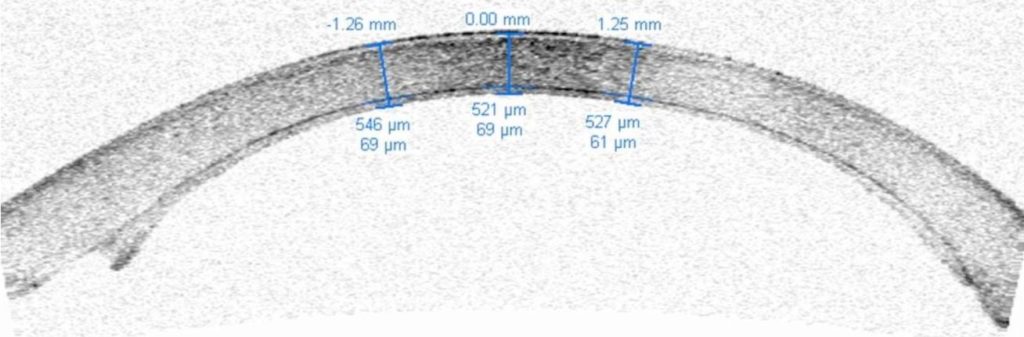
Full thickness or Penetrating keratoplasty (PK). You will undergo a thorough ophthalmic examination including advanced scanning or mapping of your cornea using the Pentacam HR or Zeiss Atlas system. You will then be in a position to make a fully informed decision as to which type of procedure will be the best for you. David Anderson introduced DSEK surgery to University Hospital Southampton in 2007 and has been at the forefront of corneal surgery since his appointment as Consultant in 2003.
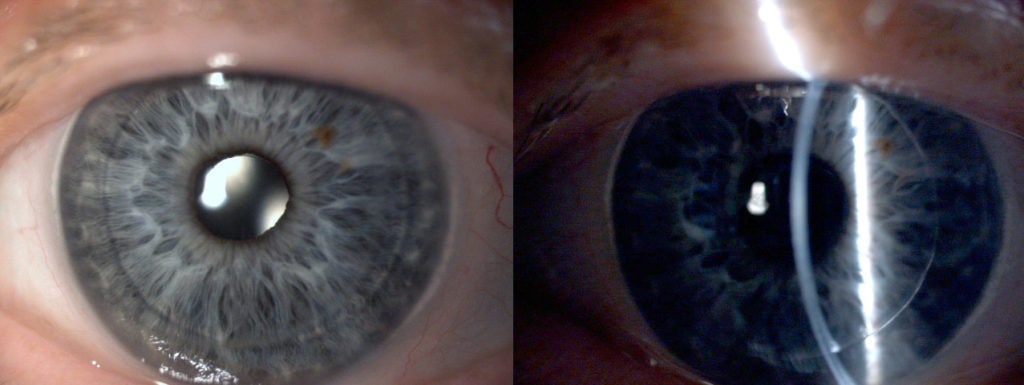
Descemet Stripping Endothelial Keratoplasty (DSEK) is a procedure designed to replace corneal endothelial cells lost through genetic disease e.g. Fuchs’ Dystrophy or following trauma from previous surgery i.e. pseudophakic bullous keratopathy.
Further information and guidance is also available on the NICE website here.
During DSEK the damaged inner layer of endothelial cells along with its supporting tissue, Descemet’s Membrane, is removed from the eye through a small entry port millimeters in size. A new layer of cells along with its supporting membrane as a small disc between 8-9mm in diameter and around a tenth of a millimeter thick is precisely created from a donor cornea. This disc is rolled up and then using a special injector, inserted into the eye through the same entry port and carefully unrolled and positioned against the underside of the cornea. An air bubble is used to help press it in place. The cells begin to pump fluid from the swollen cornea immediately which starts to stick the new sheet of cells into place. The small air bubble is left in the eye to support the new sheet whilst they continue to heal firmly into place, this air bubble will dissolve naturally in the eye over the next few days. Rather than the 16 stiches required to hold a PK in position, only one stich is required and this is usually removed at the second follow up visit a month or so later. DSEK has important advantages over PK for conditions that cause endothelial failure; the eye is more stable, quicker to recover vision, more resistant to injury and the change in spectacle prescription is far lower in turn speeding the recovery of functional vision. For these reasons and others, selective endothelial replacement surgery has become the ‘gold standard’ to treat causes of endothelial failure.
Surgery typically will take place under local anaesthesia although general anaesthesia can also be used. On the day of your procedure you will be admitted to a private room with an en-suite facility. Following administration of your anaesthetic the procedure will typically take around 40 minutes to complete. On return to your room we will ask you to lay relatively flat looking up at the ceiling for some hours so that the air bubble can continue to float upwards and push against the new layer of cells. You can sit up or stand for brief periods of time e.g. to take meals but then we will ask you to lay flay again . Your vision will be blurry because of the air bubble but this will dissolve naturally over the next few days. Most people choose to stay overnight and return home the next day although you do not have to.
Your eye may feel a little gritty or achy immediately following surgery but it should not be painful and we will place a clear shield over the eye at the time of surgery so that it is protected. We will ask you to use eyedrops frequently in the immediate post-operative period, then slowly reduce the frequency of drops over the next months, you will not need to take anti-rejection tablets unless there are exceptional circumstances. For the first day or two we ask you to lay flat as far as possible whilst the air bubble is still present. Your vision will be blurry although most people are not aware of seeing the air bubble, we ask you to arrange transport home from the hospital as you should not drive. We recommend that you avoid strenuous lifting or activity for the next few weeks following surgery and take care to avoid injury e.g. wear eye protection if gardening or playing sports like badminton or squash. As the new layer of endothelial cells continue to clear your cornea your vision will improve.
Corneal transplants are the most successful solid tissue transplant and rejection or failure of the donor material when surgery is otherwise routine is rare. Around 60-90% of transplants in the best circumstances e.g. Fuchs’ dystrophy will survive 5 years following surgery. We report a survival rate of 100% at 2 years from national audit. The longest outcomes studied to date are from the Australian Corneal Graft Registry and show that between 60 and 90% of transplants are functional at 10 years.
Rejection can occur however, so we ask you to use anti-rejection eyedrops and to report any symptoms of rejection immediately.
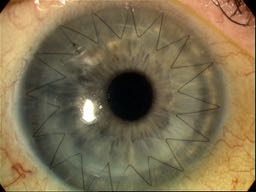
Penetrating Keratoplasty (PK) surgery was first performed in 1905 and so has been a very well characterized procedure. PK involves replacing the full thickness of the damaged cornea with a healthy disc of tissue from a donor cornea around 8mm in diameter. The new cornea is held in place with fine stitches, each around a quarter the diameter of a human hair and buried within the cornea so that they cannot be felt. As the cornea contains no blood vessels, healing between the donor and recipient cornea is slow and takes many months to years so it is important to avoid injury to the new cornea.
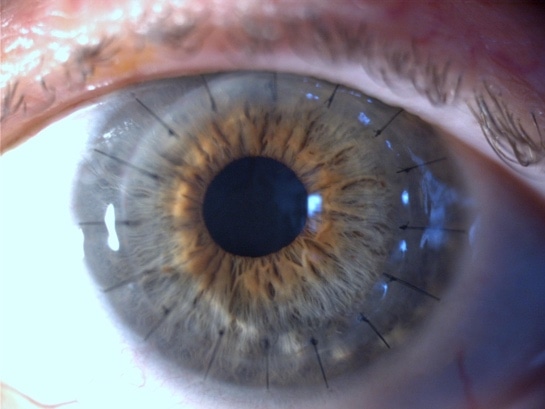
Surgery typically takes place under general anaesthesia. The procedure will typically take around one hour and afterwards your eye will feel slightly scratchy but otherwise comfortable. You will not need to stay in hospital overnight but we will arrange a follow up review within the first week following surgery.
We will ask you to use drops very frequently for the next few days, then slowly reduce the frequency over many months. You can return to normal activities but must be careful to avoid injuring your eye. We will ask you to wear protective goggles overnight. You will have blurred vision immediately following surgery and vision will slowly improve over the following weeks to months. You will need to arrange transport home from the hospital.
All operations carry the risk of complications whether from the anaesthetic, surgical procedure itself or subsequent medical procedures but these risks remain low. In addition to the risks of transplant rejection or failure, PK is an intra-ocular operation so although low, the risks of this type of surgery include the risks of any procedure performed inside the eye and include: infection, macula oedema, raised pressure of the eye and retinal detachment.
Deep anterior lamellar keratoplasty (DALK) is a variation of PK where instead of all layers of the cornea replaced with a disc of donor tissue, the epithelium and stroma are replaced leaving the original endothelium.
DALK is particularly useful for treating conditions which affect only the front layers of the cornea, too deep for laser resurfacing. We perform DALK using two methods depending on the circumstances: traditional DALK and big bubble DALK (bb-DALK).
DALK was pioneered as a technique by Dr Gerrit Melles a Dutch Ophthalmologist practicing in Rotterdam. David visited Gerritt in Rotterdam to train in this technique and has been performing DALK from 2000 to the present time.
The process of DALK including the surgery, aftercare and results are almost identical to PK (see section above). The principle advantages of DALK over PK are that rejection is less likely and because the innermost layer of the cornea is left intact the strength of the wound is higher. The is however, an interface between the donor cornea and the recipient cornea which can cause increased light scatter so final visual performance may be less clear tan with PK.
In 2015 we published a definitive review of visual quality following corneal transplantation surgery for Survey of Ophthalmology one of the highest impact ophthalmic science journals. The review can be found here.
Nuffield Health Wessex Hospital
Winchester Road, Chandlers Ford
Eastleigh, Hampshire
SO53 2DW
© Anderson Eye Care 2020. All Rights Reserved. Made by Digital Roo.
Enter your details below to get instant access to your free laser eye surgery infopack.