When people talk about diabetes, they tend to focus on things like needles and food. But those kinds of areas aren’t the only considerations when it comes to diabetes. The condition can have an effect on our vision, too. While I personally don’t treat diabetic retinopathy (for more on that, read on), it’s an important subject to explore. After all, an estimated 4.6 million people across the UK suffer from diabetes.
So how exactly can it affect the eyes? Here’s a quick starter guide…
What is diabetes?
Diabetes is a disorder that causes high levels of glucose in the blood. This happens when insulin – a hormone that helps glucose to be broken down into energy for cells – either stops being produced by the pancreas (type 1 diabetes), or isn’t produced in sufficient quantities, or doesn’t function as it should (type 2 diabetes). Type 1 diabetes normally develops earlier in life, and is usually managed with regular insulin injections. Type 2 usually develops later in life and is more common (the NHS estimates that around 90% of all adults with diabetes in the UK have type 2); it is often controlled with changes to diet and exercise.
Are eye problems inevitable with diabetes?
No. Not everyone who develops diabetes will develop vision issues. But having diabetes does raise the risk of developing certain eye conditions, so if you have been diagnosed with the condition, it’s important to have regular check-ups and screenings for your eyes (see below).
What kinds of vision problems can diabetes cause?
Diabetes can affect vision in various ways. Raised pressure in the eye increases the risk of glaucoma (a condition that causes damage to the optic nerve). Another potential complication are cataracts (blurring caused by a build-up of protein on the lens); recent studies suggest diabetics are twice as likely to develop cataracts as adults without the condition – though the precise reasons for this are still being debated. A further major complication is diabetic retinopathy.
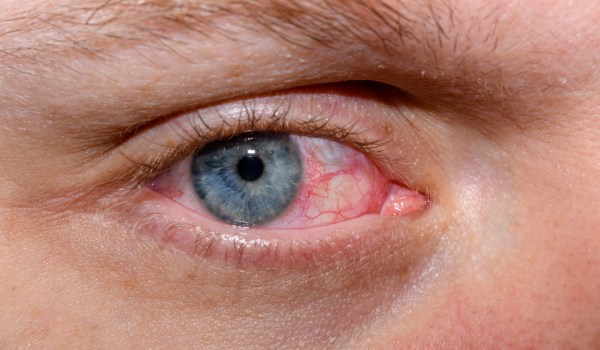
What is diabetic retinopathy?
Essentially, it involves problems with the blood vessels in the retina, and it comes in several different forms. Background diabetic retinopathy is when the capillaries (tiny blood vessels) become blocked and begin to swell or leak; this doesn’t necessarily cause noticeable vision problems, but it does need to be monitored in case the condition worsens. Proliferative diabetic retinopathy is when the blood vessels become blocked over a wider area, potentially causing reduced blood supply to the retina (known as ischaemia) and causing the body to grow new-but-weaker blood vessels (which may obscure vision if they haemorrhage). Diabetic maculopathy and diabetic macular oedema are when the central macula area of the eye becomes affected by retinopathy; these conditions can cause blurring, distortion and colour problems in the central part of vision.
How is retinopathy treated?
Diabetic retinopathy may need to be treated with laser surgery. There are two main types: localised surgery uses the laser to seal blood vessels, reduce swelling and stop bleeding. Pan-retinal surgery treats a larger area of the retina, and helps to prevent new blood vessels from growing. Laser treatment is also used for certain kinds of macular retinopathy, though injections and vitrectomy surgery (a procedure that replaces cloudy liquid in the eye with clear liquid) may also be recommended.
What can I do to help my eyes?
Some eye problems are of course simply unavoidable – but if you are diabetic, there are a number of things you can do to reduce the risk of complications. ‘Managing’ the blood is one important tool: by following your doctor’s advice to control glucose levels, blood pressure and cholesterol, you’ll be giving your eyes the best chance of staying healthy. This goes for general health, too; type 2 diabetes has a strong link to obesity, so your doctor may recommend losing weight. And it goes without saying that, if you smoke, you should strongly consider giving up: smoking increases blood pressure and raises the blood sugar level, both of which are bad for retinal blood vessels.
If you had one piece of advice…?
Have regular check-ups! Early detection is very important when it comes to treating diabetes-related eye problems, so if you have been diagnosed with the condition, make sure you keep going to your screenings (which looks for changes in the eyes that can indicate problems), as well as your regular eye checks – even if you aren’t experiencing problems at the moment. As the Royal National Institute of Blind People (RNIB) puts it: “Most sight loss from diabetes is preventable if treatment is given early. The earlier the treatment, the more effective it is.”
Medical Disclaimer
This article is for information purposes only and should not be considered medical advice. If you or any other person has a medical concern, you should consult with your health care provider or seek other professional medical treatment. Never disregard professional medical advice or delay in seeking it because of something that you have read on this blog, website or in any linked materials.