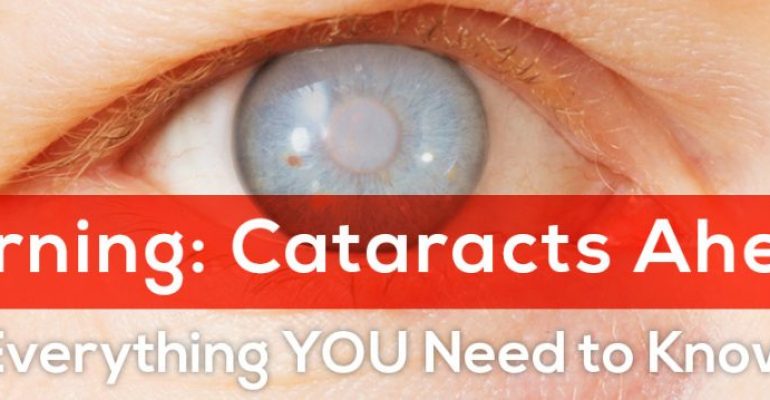
Cataracts are very common: so what are the classic signs that they might be on the horizon? And what can you do about them?
This is a blog that starts with a 19th century painter.
What does a long-dead artist have to do with a cataract blog? Stick with me. All will become clear…
You’re probably aware of JMW Turner (1775-1851). He’s a wonderful artist – a great master of oil and watercolour, often credited as a forefather of Impressionism.
Cataracts may even have sown the seeds of Impressionism.
Biographically, one of the interesting things about Turner is that his failing eyesight appears to have contributed to a change of style in later life. If you look at famous examples like Norham Castle, Sunrise (c 1845), for instance, or Ulysses Deriding Polyphemus (1829) you can see how the objects in his pictures emerge from soupy blurs of colour, and that his palette often draws on vibrant yellows.
Contemporaries didn’t always see the genius underlying those wild swirls. One newspaper of the day mockingly referred to the Ulysses painting as “colouring run mad.”
Two hundred years on, however, we do have a good theory for why Turner had embarked on this dramatic shift of form: he is widely thought to have developed cataracts in the later stages of his life. And shifts in colour perception – particularly towards the yellow end of the spectrum – are one of the common cataract symptoms.
Cataracts may even have sown the seeds of Impressionism. But that’s another story! What interests me as an ophthalmologist is how we can use our modern knowledge of cataracts to identify them as they occur – and then the very best ways of treating them.
With that in mind, what are the classic symptoms of cataracts? And who do they tend to affect? Let’s explore some of the early warning signs…
You’re getting older
Cataracts, in fact, are the number one reason for vision loss in people aged over 40.
Age isn’t a symptom of cataracts, of course. But it’s what we would call a contributory factor. And it’s a big one. While cataracts can be influenced by a variety of other risk factors – an eye injury, for example, or smoking, or diabetes, or an inherited genetic disorder – natural ageing is the most common cause of cataract development. Cataracts, in fact, are the number one reason for vision loss in people aged over 40. What’s happening is this: as we get older, the crystalline lens in our eyes starts to lose its flexibility. A young child’s lenses will be crystal clear and extremely soft, almost like a liquid gel. Once you hit your mid 40s or 50s, however, the proteins change their structure. They lose their elasticity and the tissue can begin to ‘clump’ together. In time, this build-up of tissue causes foggy, cloudy patches on the lens: cataracts.
You’re struggling to read
People often resign themselves to poor eyesight in later life, but they shouldn’t
Here’s the first of our classic symptoms. Quite often I find that cataract patients have been struggling with their reading for some time. That’s because cataract development is a gradual process. And, naturally, we don’t like to admit that our eyesight is deteriorating – even to ourselves! Cataracts will make the text in books seem blurry. You will find yourself reaching for the Increase Font Size option on your e-reader, or turning up its backlight. But at the same time you’ll probably also be struggling with text that’s further off – the subtitles on television, for example. People often resign themselves to poor eyesight in later life, but they shouldn’t. Eyes don’t wear out in the way that, say, bones or cartilage do. If you have otherwise healthy eyes, you should be seeing 20-20 when you’re 90. You should have clear vision. And if it’s not clear, there will be a reason for that.
You’re not driving at night
The glare from car headlights becomes a real problem.
“It’s fine to drive during the day,” people often say to me. “But these days I avoid the car after dark.” For an ophthalmologist, that’s another cataract red flag. Think of a cataract as a kind of yellowy (or even brunescent, ie brown) filter on the lens of your eye. In a high contrast environment – such as broad daylight, or a black-and-white eye test chart – you may not notice the difference. Deploy that filter in darker conditions, however, and your contrast clarity will drop significantly. There’s a particular type of cataract that can make that problem even more stark. A Posterior Subcapsular Lens Opacity – PSCLO for short – is a cataract that forms on the back surface of the lens. Being right next to the eye’s nodal point, a key area of refraction, it has a tendency to scatter light around the eye. The glare from car headlights becomes a real problem. Hence the night-time driving problems.
You’re losing focus on objects
Amateur golfers may find something similar going on at the tee.
Alongside the blurry words and the night-time glare comes a loss of distance-focus. Once upon a time, someone waved at you from across the street and you identified them easily. Now you look up and have to squint. Is that Mr Brown? Or could it possibly be Mrs Brown? (Or is it the Browns’ dog, Cecil?) Amateur golfers may find something similar going on at the tee. Where once they were able to track the flight of the ball without difficulty, now they’re struggling to pick it out against the sky, and where it lands. They’re losing contrast because the cataract is clouding the once-clear line of vision. Imagine teeing off into a Turner painting, if such a thing were possible; the ball would be rather tricky to identify!
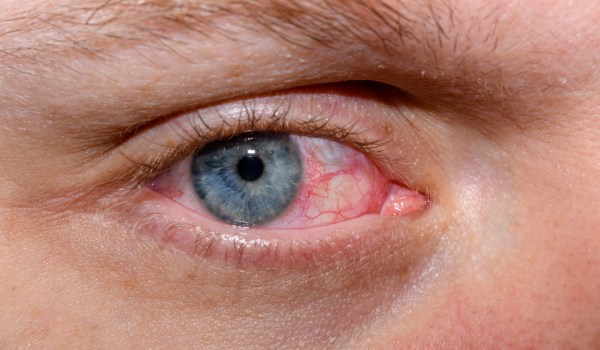
You’re seeing halos
A more common reason is a cataract
By halos, we mean a circle that appears around a light source: a faint ring around a street lamp, for example. There are a number of reasons why you might see halos where there aren’t any. One of the more serious reasons is acute glaucoma, where the optic nerve becomes damaged. But a more common reason is a cataract, which creates a sort of diffuse blur around bright lights. As with night-time driving, it’s refraction changes that are causing the issue. Where once light travelled to your retina unimpeded, now it’s hitting that ‘filter’ and scattering in strange new ways. Diplopia, better known as double vision, is a related symptom; typically, the cataract in one eye causes objects to double up, affecting your vision accordingly.
So how do we treat them?
That’s quite enough bad news about cataracts. Now for the good news! And the best news about cataracts is that they are very treatable. So treatable, in fact, that cataract surgery is now the most commonly performed operation in the UK, with over 300,000 procedures undertaken every year. It’s also very quick to perform: a normal cataract operation lasts for 15 minutes or less. We use fast-acting drops rather than injections to numb the eye (though general anaesthetic is available for patients who prefer to be unconscious during the procedure, and mild sedation for those who might prefer to be awake but in a more relaxed state of awareness). And post-operation discomfort tends to be minimal; most people say their eyes feel a little achy or ‘gritty’ after surgery, but these irritations can usually be dispatched with a paracetamol. Another great thing about cataract surgery is that it can be done at almost any time. You may have heard it said that cataracts need to be ‘ripe’ before becoming operable. That used to apply but, thanks to the advances in modern surgery, it’s no longer a factor. These days I advise patients with early-onset cataracts to fix them whenever the symptoms start to impinge on daily life. That might be at the very first appearance of symptoms like the ones above. But the decision differs from patient to patient.
One thing is for sure, however: you don’t need to struggle along with vision problems like poor old Turner did. Bad news for fans of visionary oil painting, perhaps – but good news for everyone else.
Medical Disclaimer
This article is for information purposes only and should not be considered medical advice. If you or any other person has a medical concern, you should consult with your health care provider or seek other professional medical treatment. Never disregard professional medical advice or delay in seeking it because of something that you have read on this blog, website or in any linked materials.